Fibroblasts are ubiquitous cells that were initially described as immunological inert bystanders just responsible for the production and remodeling of the extracellular matrix (ECM).
Their role in health and disease is, however, much more multifaceted and complex. Fibroblasts are significantly involved in maintaining tissue-specific immunity by activating local immune responses upon detection of pathological stimuli. After clearance of the pathogen, they orchestrate resolution of inflammation by reducing and discontinuing their support for immune cells. Recent research shows that inappropriate and or sustained fibroblast activation promotes persistence of inflammation, ultimately resulting in tissue damage and organ failure. Knowledge of the mechanisms underlying the aberrant activation of fibroblasts in chronic inflammatory diseases, will help to develop innovative therapeutic approaches.
Our lab is particularly interested in rheumatoid arthritis (RA) pathogenesis. RA is a chronic inflammatory disease that mainly affects the joints. Abnormal activation of fibroblast-like synoviocytes (FLS), which are resident cells of the synovial membrane, is key for sustained immune cell activation (within the synovial membrane) and drives the destruction of the articular cartilage and bone. By using traditional biochemical assays (e.g. western blots, ELISA,…) and advanced sequencing technologies we aim to gain a better understanding how inflammatory and metabolic pathways interact to promote FLS activation. We further use innovative high content imaging screening efforts to study FLS and immune cell interactions and how these pathogenic interactions can be targeted to develop novel therapeutic strategies that can stop chronic synovial inflammation.
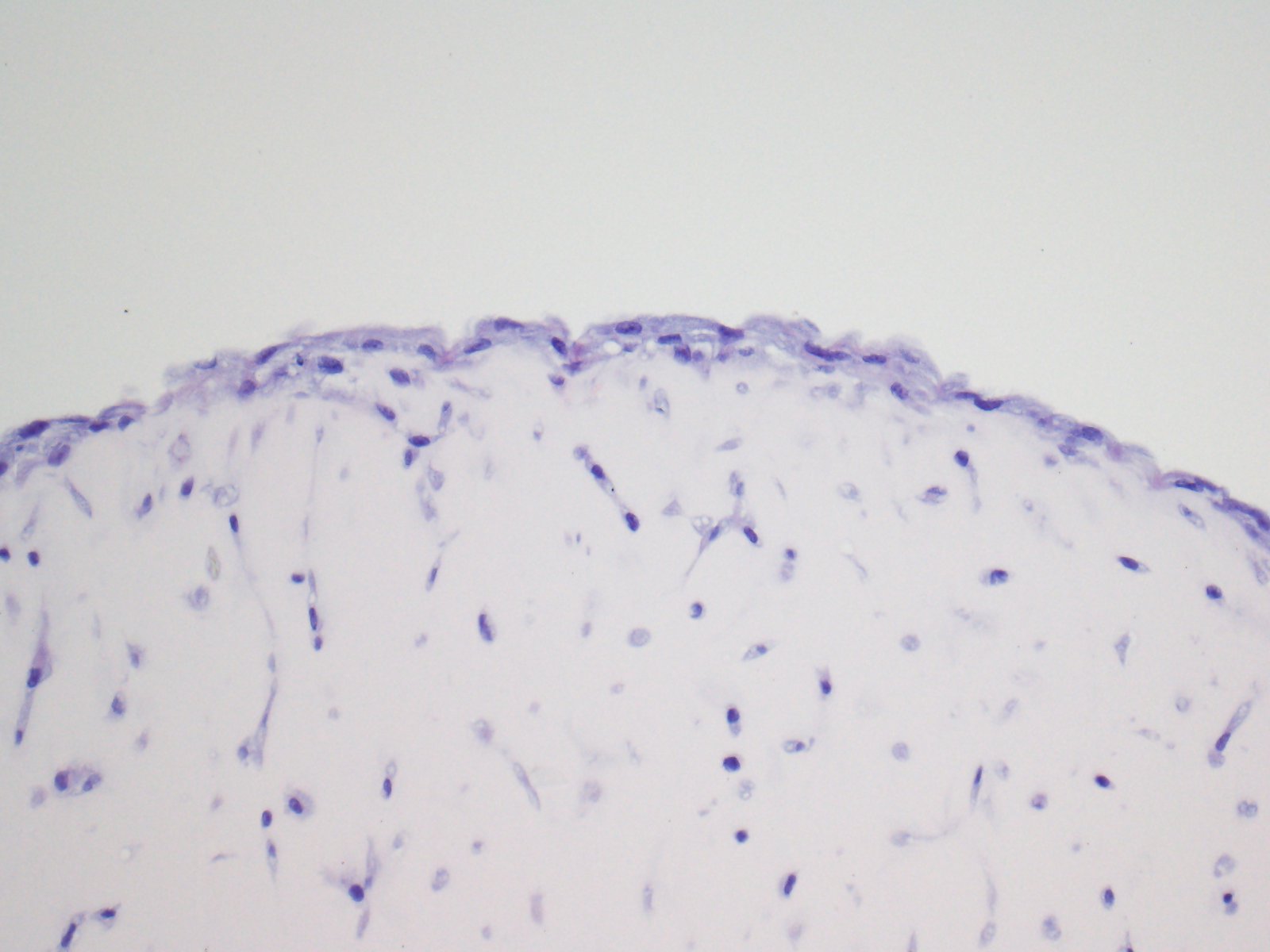

On the left, an IHC picture showing FLS in a 3D synovial organ culture system. On the right, an IF picture showing FLS-T-cell interactions in vitro.
Publications Highlights
Cytokine-directed cellular cross-talk imprints synovial pathotypes in rheumatoid arthritis.
In this study we characterize T-cell-FLS interactions in the context of RA by using a high content imaging platform. We further show how distinct inflammatory cytokines specifically impact these interactions and translate our in-vitro findings in clinically relevant synovial pathotypes of RA.
/!\ Watch our dedicated video on this link.
TNFR2 is critical for TNF-induced rheumatoid arthritis fibroblast-like synoviocyte inflammation.
Our work here demonstrates the crucial role of TNF-receptor 2 (TNFR2, TNFRSF1B) in FLS activation in the context of RA.
IRF1 is critical for the TNF-driven interferon response in rheumatoid fibroblast-like synoviocytes.
Within this paper we establish a role for the transcription factor IRF1 in TNF-induced activation of RA-FLS. We further describe a TNF-IRF1-STAT1 signaling cascade that is important for FLS chemokine secretion.
mTOR Senses environmental cues to shape the fibroblast-like synoviocyte response to inflammation.
In this paper we show how the metabolic mTOR pathway senses and shapes the cellular response to inflammatory stimuli, such as TNF. We further show how the metabolic microenvironment impacts on the FLS response to inflammation via mTOR.
