Imaging allows us to blink under the surface of arthritis and rheumatic disease.
The most common manifestation of musculoskeletal disease is arthritis, which has many causes, faces, and impacts both those affected and their carers. Over the past decade, emerging musculoskeletal imaging techniques have become indispensable tools both in clinical practice and in research in rheumatology. While conventional radiography is performed generally by radiologists (but interpreted also by rheumatologists) modern imaging methods, i.e. musculoskeletal ultrasound, magnetic resonance imaging, computed tomography, and positron emission tomography are increasingly utilised and interpreted by rheumatologists.
Ultrasound machines are commonly applied as diagnostic and monitoring tools in rheumatological departments and private practices. While positron emission tomography, computed tomography and magnetic resonance imaging are generally operated and performed by radiologists, there are dedicated units in individual rheumatological centres solely under the control or catering specifically to the needs of rheumatology departments. These techniques enable the in-depth visualization of both inflammatory changes, which are the common denominator of rheumatic and musculoskeletal diseases, but also of the ensuing structural damage, which leads to functional disability and decline in patients.
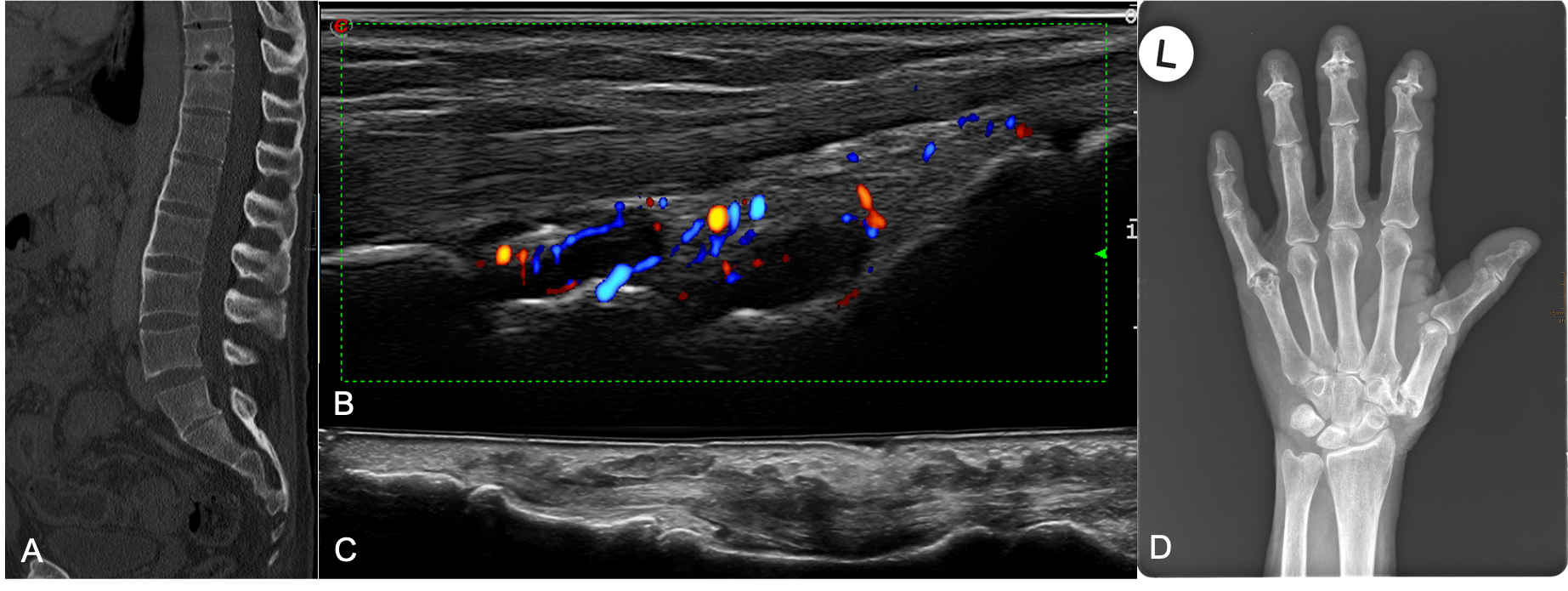
Multimodal imaging in psoriatic arthritis. A. Magnetic resonance imaging of the spine showing syndesmophytes, shiny corners and Andersson lesion. B. Ultrasonography of the dorsal aspect of the wrist showing synovial effusion, hypertrophy and Doppler signal around the radiocarpal and intercarpal joint. C. Ultrasonography of the volar aspect of a finger showing tenosynovitis of the flexor tendon. D. Conventional posteroanterior radiograph of the hand showing marked severe destruction of the scaphotrapeziotrapezoidal joint, as well as pencil-in-cup lesions of the fifth metacarpophalangeal joint, distal interphalangeal joints 4 and 2 as well as joint space narrowing and ostephytes of all proximal- and distal-interphalangeal joints.
The main focus of our group focuses on investigating the utility of these methods, both as ideal tools for clinical practice and as outcome measures for research. Work performed by our group has led to the recognition of the Division as a member of the EULAR Network of Imaging Research and Training centres. Part of our research focuses on inflammation, structural damage and fibrosis, and the ability of various imaging techniques such as ultrasound or positron emission tomography to depict such changes.
Building on our endeavours in this area, we recently began to pursue diagnostic applications also in basic research, and as part of joint grant are currently developing aptamers, single-stranded oligonucleotides capable of specifically binding to target proteins on various cells, among them synovial fibroblasts, the key cells responsible for both joint destruction in arthritis but also for fibrotic diseases across a range of medical disciplines. To allow this translational research to flourish, our group, along with contribution from other colleagues has played a fundamental role in the establishment of ultrasound-guided synovial biopsies at the Division.
Latest Research
Systematic literature review to inform the EULAR recommendations for the use of imaging in crystal-induced arthropathies in clinical practice. Ann Rheum Dis. August 2024
Watch our dedicated video here.
2023 EULAR recommendations on imaging in diagnosis and management of crystal-induced arthropathies in clinical practice. Ann Rheum Dis. May 2024
Watch our dedicated video here.
